If you are taking the right dose of thyroid medicine, and perhaps are even getting adrenal support, but still have many hypothyroid symptoms you may have Reverse T3 (RT3).
This information came from the experiences of other patients on the RT3 Yahoo Group and specifically patient Nick Foote who did some great work compiling a Question and Answer site about Reverse T3 (RT3). Please read the entire page for important information and cautions.
What is “Resistance” caused by Reverse T3?
“Resistance to thyroid hormone” refers to people that don’t respond properly to thyroid hormone supplementation (such as natural desiccated thyroid medicine like Naturthroid or Erfa), and continue to have hypothyroid symptoms and normal blood test results.
Why does this happen?
It helps to first understand the relationship between the thyroid hormones T4 and T3 in the body. T4 is the main hormone that is produced by the thyroid gland. This hormone is totally inactive biologically. It’s only after an iodine atom is removed, making it into T3, that it has an effect on the body. T4 is a storage hormone and lasts for weeks in the body. T3 has a life of a few days in the body, but it is the important catalyst that the body needs to progress at the right speed. Without enough T3 people experience Hypothyroid symptoms (cold, tired, and lethargic, etc..).
Reverse T3 (RT3) is what is made when the “wrong” iodine atom is removed from T4 which results in blocking the action of T3 on the body. This means that your body doesn’t respond properly to T3 leading to hypothyroid symptoms despite a normal TSH, T3 and T4 lab levels.
This is what they refer to as “Tissue Resistance to Thyroid Hormone.” According to Nick Foote’s website, doctors will say this is very rare, but that’s because they don’t look for it!
What are the symptoms of Reverse T3 (RT3)?
Hypothyroidism that won’t respond to desiccated thyroid treatment (at a proper dose). It may sound similar to Chronic Fatigue Symptom.
Unless you have a very clued in Doctor this disgnosis will probably get missed. It can by picked up by blood tests, but only if they do the right ones and then interpret the results correctly.
How is Reverse T3 (RT3) diagnosed?
The initial sign tends to be that normal thyroid treatment doesn’t work. Other signs of possible RT3 problems are low but stable temperature, Ferritin of at least 70, Free T3 (FT3) near the top of the range (which varies by lab).
RT3 can be accurately diagnosed by calculating the ratio of Free T3 to Reverse T3 from your lab results. Simply divide the Free T3 number by the reverse T3. It should be 20 or greater. If the ratio is less than 20, its very likely you have an RT3 problem. Please note: lab ranges vary so look at the ratio instead.
If you only had a T3 lab test (but not a FT3), then divide the T3 by the RT3 result. The ratio should be 10 or greater. Less than 10 likely means an RT3 problem.
A FT4 reading that is over 1.4 is a marker for potential high RT3.
What causes Reverse T3 (RT3)?
The body naturally produces some RT3 and this is fine for many people. The problem arises when the Free T3 to Reverse T3 ratio is too low (below 20:1) because the RT3 then gets in the way of the T3, causing hypothyroid symptoms. Here are some common causes for a low FT3/RT3 ratio:
- Extreme dieting, the RT3 increases to slow the metabolism and make better use of the available food
- Low Ferritin
- High cortisol, this disturbs the balance of the thyroid hormones
- Low cortisol, this again disturbs the balance of the thyroid hormones
- Insulin dependent Diabetes
- Low Vitamin B12 levels
How is Reverse T3 (RT3) treated?
The treatment for too much RT3 first involves stopping more RT3 being made and waiting for the RT3 already in the body to decay or be excreted.
This is relatively easy but there are pitfalls along the way. A lot of Drs are worried by people doing this as things happen too quickly to be done by lab tests. Patients need to adjust the dose by symptoms and vital signs.
RT3 is only made from T4. If you get rid of T4, both from your own thyroid and from supplements, then no more RT3 gets made. In order to do this and stay alive an alternative source of the bio-active T3 is neededthrough synthetic T3 hormone.
The basic treatment is to stop all medicine containing T4 (such as Naturthroid, Armour, Erfa, etc..) and start T3 medicine instead. Slowly increase the dose of the T3 medicine week by week as the T4 levels in your body diminish. After about 6 weeks, the T4 and RT3 levels in your blood will be very low. It takes about a total of 12 weeks for the RT3 to clear the receptors.
During this time, its very likely you will experience Hypothyroid symptoms. To help with this you can increase the T3 medicine levels but be prepared to drop the dose as soon as the thyroid resistance clears because this can happen dramatically and suddenly. Overnight you may very well have to drop you T3 medicine dose almost completely. Then ramp back up to about half the previous dose until you stop feeling hypothyroid. So its very important to carefully watch symptoms, including pulse and body temperature, especially around week 12.
(If you are worried about this you can keep the T3 dose lower but it means feeling hypothyroid until the RT3 clears. If you need to get on with life and can’t afford to stay hypothyroid for another the three month clearing time, then increase the T3 dose as noted above).
What lab work do I need?
Lab work has a lot of value to it but needs to be interpreted carefully, just because the results are “in range” doesn’t mean you will feel well, they need to be in the right part of the reference ranges. There are some excellent resources on lab work, including many that you can order without needing a Doctor. See STTM Lab page.
RT3 and FT3 tests can be ordered without a doctor and there are sources of this in the Yahoo RT3 group files area for members. IMPORTANT NOTE: To calulate the RT3 ratio, the Free T3 and RT3 lab work has to be done at the same time.
Econolabs and Life Extension are currently the cheapest sources for RT3 testing.
What is T3 medicine?
T3-only medication include brand names like Cytomel (American), Cynomel (Mexican), or Tertroxin (UK). The Chemical names for this are Liothyronine sodium or triiodothyronine. See Wikepedia for more information
What if I am already on Thyroid medicine?
If you are on synthetic T4 medication such as Synthroid, or Natural Desiccated Thyroid such as Armour, Naturthroid or Erfa, these all contain T4. During the 12 weeks or so that you clear the RT3 from your body, you will need to change your medication to a T3 only medicine (noted above).
Do I want/need Sustained Release T3 (SRT3)?
According to Nick Foote’s site, no, sustained release is not necessary.
Do I need T4 at all?
When it comes to RT3 people, NO, T4 is not needed. For these people, T3 only is the protocol. There are people who have been on T3 only for 20 years without ill effects.
DANGERS, Please read!
Once you are on T3 only it important to stay on it, or if you are switching medicines to change very gradually. If you suddenly stop taking T3 you could be in a myxadema coma within 24 hours. Its well worth carrying a medical warning note that you are on T3 only and the dosage in case you are rendered unconscious in a car accident.
Stopping Meds before Lab Tests
When performing lab tests you sometimes need to stop your medication before the blood draw. This is a list of the common withdrawal periods. Unless specified otherwise you only have to stop taking the hormone being tested for.
Thyroid Medicine
Don’t take any thyroid medication on the day of the blood draw. Consider not taking any T3 after lunchtime the pervious day, especially if your Dr gets concerned by over range FT3. You can take your HC as normal on the day of the blood draw if you are on it.
Cortisol/Adrenal Support
The “gold standard” for Adrenal hormones is the “4 times a day saliva test”. If you have taken any cortisol (HC), Isocort or had Licorice 2 weeks before testing the results will be inaccurate.
Sex Hormones
If you are supplementing sex hormones using creams applied topically then saliva tests are not accurate. Blood tests remain accurate if you are supplementing but none should be taken on the day of the test.
Ferritin/Iron Panel
Stop all iron supplements 5 days prior to blood draw.
Where can I get more help on Reverse T3?
Join the 1200 members on Yahoo’s RT3 group.
AUTHOR’S NOTE
Please note, I do not suffer from RT3 (at least from what I know) but wanted to share this information from Nick Foote’s site because it seems so important, and everyone is different. Good luck!








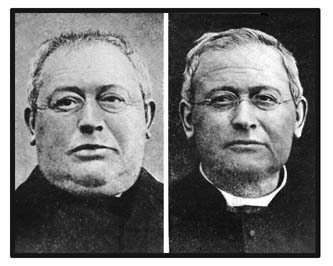 Adult Male, Before and After Treatment
Adult Male, Before and After Treatment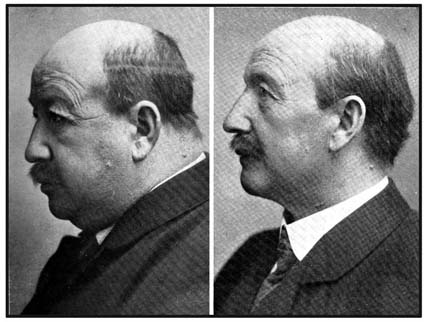 Adult Male, Before and After Treatment
Adult Male, Before and After Treatment
 This time of year is always tough for me. The days are getting longer, there is more light and I feel like I should be feeling great. But sure enough, I feel the
This time of year is always tough for me. The days are getting longer, there is more light and I feel like I should be feeling great. But sure enough, I feel the